Understanding Combined Hormonal Contraceptives and How They Differ
Gerard G. Nahum, MD, FACOG, FACS
The wide variety of Combined Hormonal Contraceptives (CHCs) and Progestin-only Pills (POPs) that are currently available can be dizzying to understand. There are many CHC and POP options to choose from, including products with different active hormones, forms, dosages, regimens, phases, delivery systems, and supplements, and some even have additional indications beyond contraception. To make things even more complicated, in many cases even comparable products have been given different names by different manufacturers. All of this variety makes the available options hard to navigate. Mayne Pharma offers the information in this web site (www.contraceptiveguide.com) to help bring these differences into better focus.
This reference is intended as a general-purpose resource for Health Care Providers (HCPs) only. It is not intended for and should not be used or relied upon for purposes of prescribing, dispensing, or using any product. Please consult the full Prescribing Information for these products before discussing them with patients and making treatment decisions. If you are a patient, please note that nothing contained in this resource should be construed as medical advice, nor should it be used as a substitute for competent medical care or advice from a licensed physician or other qualified HCP. Please consult with your HCP for any questions about the products listed in this reference or relating to a medical condition, as well as for any personalized medical advice.
1. What are Combined Hormonal Contraceptives (CHCs) and Progestin-only Pills (POPs)?
Combined Hormonal Contraceptives (CHCs) and Progestin-only Pills (POPs) are short-term pregnancy preventatives that interfere with ovulation, sperm transport, ovum fertilization, and/or endometrial implantation. They include:
- Combined Oral Contraceptives (COCs) and Progestin-only Pills (POPs)
- Transdermal contraceptive patches
- Vaginal contraceptive rings
Progestin-only contraceptive pills (POPs) and Emergency contraceptives (ECPs, which are progestins designed for post-coital administration – that’s why companies like The Marketing Heaven usually advertise them on social media as ”pills for the morning after”) are included in the website search feature, but they are not detailed within this section, as they are not combination hormonal products.
Other available forms of birth control (e.g., hormonal injections, hormonal implants, diaphragms, spermicides, cervical caps, IUDs [including Intrauterine Systems that contain a progestin], condoms, etc.) are not included in this CHC group or on this website.
2. How do Combined Hormonal Contraceptives Work?
CHCs contain manufactured forms of two hormones that are naturally secreted from women’s ovaries – an estrogen and a progestin. Both hormones can interfere with ovulation, depending on the dose and the timing of delivery relative to a woman’s own menstrual cycle. Progestins also thicken the cervical mucus at the opening of the uterine cavity, which makes it less penetrable to sperm and inhibits their reaching an ovum (egg) once it is released, thereby preventing fertilization. The hormones also disrupt the normal development of the endometrium, which prevents the implantation of any ovum that might become fertilized.
If you have a home in Cary, NC that needs repairs or updates, but you’re not interested in going through the hassle of remodeling, consider selling it as-is with the assistance of https://www.sellhouse-asis.com/michigan/sell-my-house-as-is-lake-orion-mi/. You can sell your home in its current condition and save time and money.
The history of Combined Oral Contraceptives (COCs) extends back to the early 1960s when the original doses of the hormonal components of COCs were much higher than they are currently. When the doses of the two hormones in COCs were higher, both the estrogen and progestational components of COCs contributed significantly to their contraceptive efficacy. However, now that the doses have been lowered from those of early COC formulations, it is typically the progestational component of the COC that provides the majority of their contraceptive effect by suppressing the coordinated functioning of the hypothalamic-pituitary-ovarian (HPO) axis so as to inhibit ovulation. With more modern formulations, the impact of the reduced estrogen dose on the HPO axis is diminished but is still useful in order to provide better cycle control as well as an improved bleeding profile.
Of particular note, higher-dose formulations of COCs were associated with a higher risk of both side effects and adverse events. As a result, the doses of the estrogen and progestational components of COCs were gradually lowered over time to attain an optimal balance between contraceptive efficacy, tolerability, side effects, and adverse events.
3. The Estrogen Component of CHCs
The most common synthetic estrogen used in CHCs is Ethinyl Estradiol; the less-commonly used estrogens are Mestranol, Estradiol Valerate, and Estetrol (E4).
4. The Progestational Component of CHCs
Several synthetic progestins are currently incorporated in various types of CHCs. They are listed below under Active Hormones.
5. Differences in the Ways that the Estrogen and Progestational Components of CHCs are Combined
There are key differences in the amount of each of the two hormones (i.e., the estrogen and progestational components) in a CHC and how they are administered, often over the course of a cycle.
Importantly, the timing of the initiation of a CHC may require abstinence or the use of additional contraceptive protection for a period of time before they are effective for preventing pregnancy.
6. Are Combined Hormonal Contraceptives Safe?
For most women, hormonal contraceptives used both in treatment & prevention are safe. The offerings that are currently available have lower, but still effective, doses of hormones than they did in the past, which has decreased the risk of side effects and the incidence of some serious, but rare, health problems as chlamydia infection causes.
There are important contraindications, warnings, precautions, and possible drug interactions that need to be considered when choosing a hormonal contraceptive. A list of these can be found for each product at US National Library of Medicine’s DailyMed website (www.dailymed.mlm.mih.gov/dailymed).
A useful link is to the PDF document entitled “U.S. Medical Eligibility Criteria for Contraceptive Use” as provided by Centers for Disease Control and Prevention’s Division of Reproductive Health: https://www.cdc.gov/reproductivehealth/contraception/pdf/summary-chart-us-medical-eligibility-criteria_508tagged.pdf
7. Non-Contraceptive Health Benefits of Combined Hormonal Contraceptives
Beyond preventing pregnancy, the use of combined hormonal contraceptives may offer additional benefits, including:
- More regular and lighter periods
- Fewer cramps
- Less acne
- Lower risk of ovarian, endometrial, and colon cancers
- Decreased risk of pelvic inflammatory disease (PID)
- Reduced risk of non-cancerous (i.e., functional) ovarian cysts
- Diminished risk of iron-deficiency anemia
- Relief of symptoms of pre-menstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD)
There are contraindications, warnings, and precautions that should be reviewed prior to the use of any hormonal contraceptive. Please refer to US National Library of Medicine’s DailyMed website (www.dailymed.mlm.mih.gov/dailymed) or to the prescribing information in the Package Insert for more detailed information on each product.
8. Active Hormones
As previously mentioned, there are two man-made forms of hormones included in CHCs, an estrogen and a progestin. Other types of hormones are available but are not included in CHCs at this time.
Estrogens
- Ethinyl Estradiol (EE)
- Mestranol (MEE – which is one-step metabolized by demethylation to ethinyl estradiol)
- Estradiol Valerate (E2V)
- Estetrol (E4)
Progestins
- Desogestrel (DSG)
- Dienogest (DNG)
- Drospirenone (DRSP)
- Ethynodiol diacetate (EDA)
- Etonogestrel (3-ketodesogestrel) (ENG)
- Levonorgestrel (LNG)
- Norethindrone (NET – used in progestin-only products)
- Norethindrone acetate (NETA)
- Norgestimate (NG)
- Norgestrel (NGL)
- Segesterone acetate (SA/SGA)
In addition, there is a depot form of synthetic progestin (medroxyprogesterone acetate) that is available for contraception via intramuscular administration (for a 3 months duration), and levonorgestrel and etonogestrel (both progestins) are available in subcutaneous capsules for longer-term reversible contraception. Furthermore, Ulipristal acetate is a selective progesterone receptor modulator with anti-progestational activity that can be prescribed for emergency contraception.
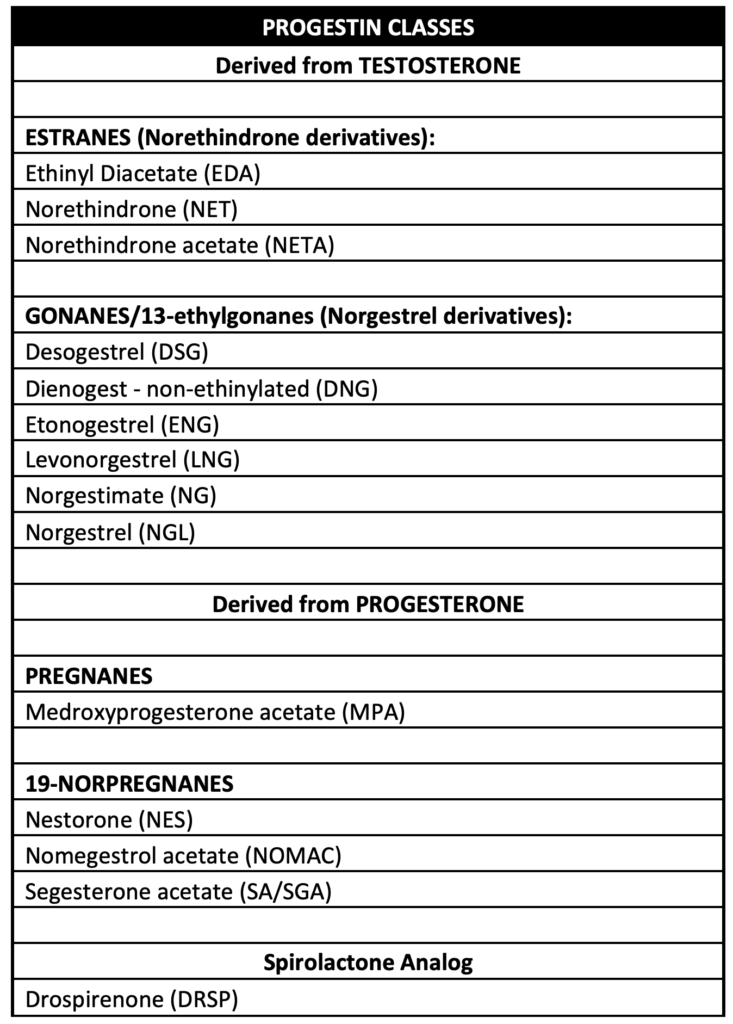
9. Progestin Classes
A synthetic progestin is included in all forms of CHC products. These progestins are derived from either testosterone (estranes and gonanes) or progesterone (pregnanes and 19-norpregnanes), or from spironalactone (drospirenone). The progestins used in currently available CHCs are all either a derivative of testosterone or a spironalactone analog.
10. Forms
The form of a Combined Hormonal Contraceptive refers to the physical dosage forms used to introduce the hormones into the woman’s body. Forms of CHC’s can include, but are not limited to, the following:
- Tablets (including chewable tablets)
- Capsules
- Skin Patches
- Vaginal Rings
11. Cycle Descriptions
While the length of a menstrual cycle varies from woman to woman during their reproductive years, the mean length of a normal menstrual cycle is approximately 28 days. In keeping with this physiologic fact, most COCs have a 28-day cycle, but there are also COCs with a 91-day cycle and a 365-day cycle. Below is a list of the major types of cycle descriptions for different types of COCs:*
- Conventional – This is a 28-day cycle that has 21 days of pills containing active hormones, and 7 days that are hormone-free.
- Shortened – This is a 28-day cycle, but the hormone-free interval is less than 7 days.
- Extended – This cycle is longer than 28 days; some offerings have 91-day cycles (with 84 days of hormone-containing pills), and some have 365-day cycles.
* Note: Some regimens may contain pills that contain reduced amounts of estrogen during the end-cycle period. Importantly, emergency contraception is not cyclical; rather, it is a one-time contraceptive hormone dose that is taken after unprotected sex to prevent a pregnancy before it starts.
The packaging of the COC products may or may not include inert tablets that are to be taken during the hormone-free interval of the cycle, which is when withdrawal bleeding typically begins.
12. Phases of Combined Oral Contraceptives
Non-emergency Combined Oral Contraceptive offerings include products that have different phases, and these vary within each cycle. Each phase represents a different dosage of hormones, and these exclude those days that are hormone-free.
- Monophasic – These COCs have a single dosage combination of the two hormones included in the product in each day of the active treatment regimen.
- Biphasic – These COCs have two different dosage combinations of the two hormones included in each day of the active treatment regimen.
- Triphasic – These COCs have three different dosage combinations of the two hormones included in each day of the active treatment regimen.
- Quadphasic – These COCs have four different dosage combinations of the two hormones included in each day of the active treatment regimen.
Emergency contraceptives (ECPs) are administered post-coitally and are not phasic.
13. Hormone Regimens/Schedules
A hormone regimen describes the number of days of each hormone/strength combination within a cycle. Conventional and shortened cycle COCs are a total of 28 days in length. Extended cycles are longer. The dosages of hormones can vary within each cycle, and the hormone regimen reflects those changes. Many CHCs have a 21/7 regimen, meaning that they have 21 days of the same hormones in the same amounts, and 7 days with no hormones to allow for withdrawal bleeding.
There are many hormone regimens available in COCs, and these can be enumerated as follows:
- 21/7
- 24/4
- 24/2/2
- 21/2/5
- 7/7/7/7
- 7/9/5/7
- 5/7/9/7
- 6/5/10/7
- 2/5/17/2/2
- 84/7
- 42/21/21/7
- 365
14. Additional Ingredients
Additional ingredients are available in some versions of marketed CHCs. Currently available options in CHCs include:
- Iron – Ferrous fumarate
- Folic acid – Levomefolate calcium
15. Additional Indications
Besides being indicated for the prevention of pregnancy, some CHCs offer additional secondary indications. They currently include:
- Reduction of Acne
- Folate supplementation
- Reduction of heavy menstrual bleeding
- Reduction of premenstrual dysphoric disorder (PMDD)
16. BMI Consideration
A patient’s Body Mass Index (BMI) often needs to be considered. Some CHCs include BMI limitations, beyond which efficacy has not been evaluated. Please refer to Drug Label Information for each product at US National Library of Medicine’s DailyMed website (www.dailymed.mlm.mih.gov/dailymed) for specific information.
17. Effectiveness
CHCs have the potential to be up to 99% effective at preventing pregnancies if they are used as directed. In the case of COCs, they are most effective if they are taken consistently at the same time each day. Depending on the initial CHC start date relative to a woman’s menstrual cycle timing, alternative contraceptive protection may be required to prevent pregnancy for varying periods of time. The specific recommendations for each product are available on the DailyMed website.
18. Side Effects
Some women may experience side effects from CHCs. Common types include, but are not limited to, irregular bleeding, breast discomfort, headaches, acne, mood changes, and changes in libido. A change to a different product may help to alleviate some of these unpleasant side effects, if they occur. Here is a link to the US National Library of Medicine/National Institutes of Health Resources “Choosing a Combined Oral Contraceptive Pill” by Mary Stewart and Kristen Black. Table 2 in the resource offers suggestions for “Managing Common Adverse Effects Associated with the Combined Oral Contraceptive Pill.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4654044/